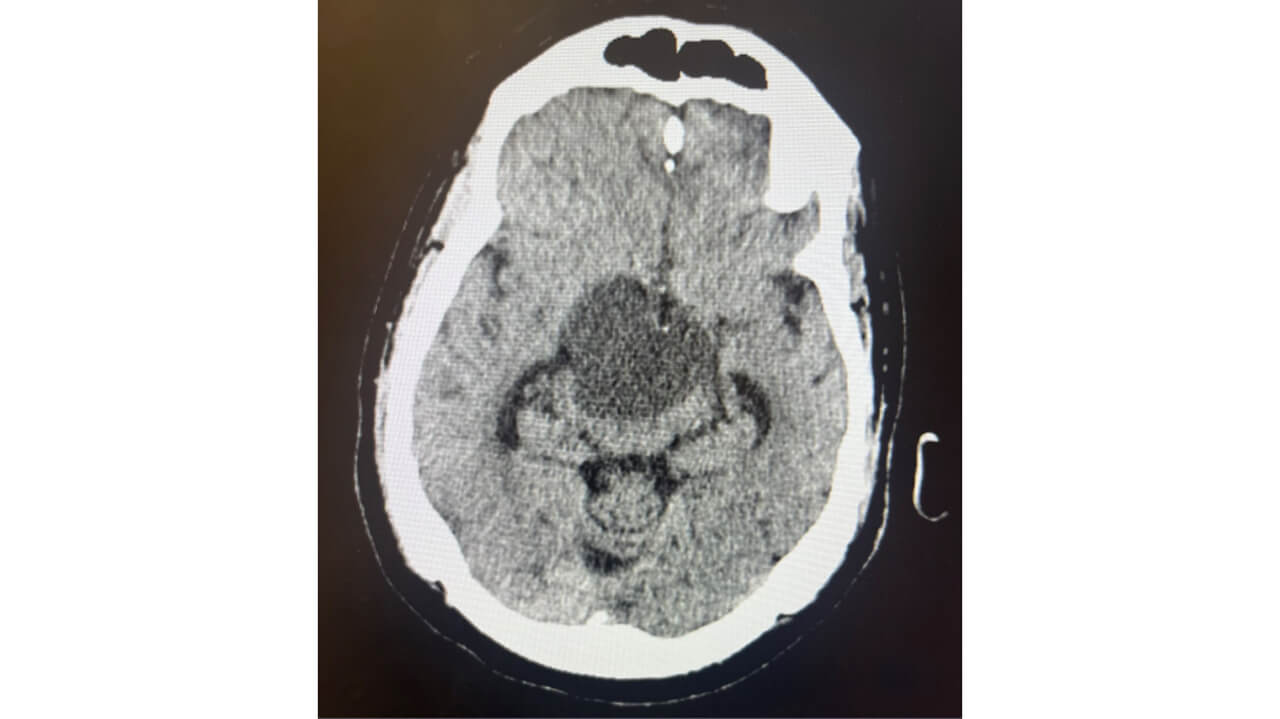
Image 1: Craniopharyngioma
Physician Assistant (PA)
Physician Assistant (PA)
This project was completed for PY 652: Medical Writing & Biostatistics for PA.
After working closely with a patient diagnosed with a craniopharyngioma, a rare benign brain tumor that accounts for approximately 0.8% of all brain tumors, April Alver '23, MHS ‘25 explored treatment approaches in the context of the patient’s clinical course, highlighting the complexities of managing recurrent disease and balancing treatment risks with long-term outcomes.

Physician Assistant
School of Health Sciences
Brief History:
Physical Exam:
Vitals:
Differential Diagnosis:
Diagnostic Results:
CT head w/o contrast 10/13 11am
CT head w/o contrast 10/13 10pm
CT head w/o contrast 10/17
Figure 1: Hospital Course
| Presented to an outside hospital from a skilled nursing facility with altered mental status and lethargy | Transferred for concern of abnormal head CT Patient was hypertensive and found to have excessive urination |
Overnight GCS decreased from 14 to 11 | Neurosurgery procedure | Discharged home with follow up plan |
Figure 2: Electrolyte and Osmolarity Lab Tests
| Lab Test | Patient’s values | Reference Range |
| Urine Osmolality | 119 mOsm/Kg | 40-1,400 mOsm/Kg |
| Serum / Plasma Osmolality | 321 mOsm/Kg | 285-295 mOsm/Kg |
| Serum Sodium | 146 mmol/L | 136-145 mmol/L |
Figure 3: Pituitary Lab Tests
| Lab Test | Patient’s values | Reference Range |
| AM Cortisol |
0.4 ug/dL (Due to missed hydrocortisone dose) |
6.2-19.4 ug/dL |
| Free T4 | 0.6 ng/dL | 0.80-1.90 ng/dL |
| Total Testosterone | <3 ng/dL | 193-740 ng/dL |
| Follicle Stimulating Hormone | 1.4 mIU/mL | 1.4-12.8 mIU/mL |
| Luteinizing Hormone | <0.2 mIU/mL | 1.6-15.2 mIU/mL |
CT head w/o contrast 10/13 10pm
Final Diagnosis:
Treatment:
Patient Outcome:
Two Week Outpatient Follow Up:
"This project has helped prepare me for a career as a physician assistant by encouraging me to push beyond my comfort zone and learn about complex and unfamiliar conditions. It reinforced the importance of continuous learning and adaptability in clinical practice. Presenting my findings at a professional conference highlighted the important role PAs fulfill not only in patient care but also in advancing research and evidence-based practice." - April Alver '23, MHS '25
This serves as an overview of the project and does not include the complete work. To further discuss this project, please email April Alver.
PY 652: Medical Writing & Biostatistics for PA introduces biostatistics, evidence-based medicine, as well as critical review and application of evidence to clinical decision-making. Students learn to construct clinical questions and perform literature searches. Methods for critically appraising the literature and strategies for maintaining currency of medical knowledge through journal clubs are practiced. Review of basic techniques of medical writing and presentation allow students to develop presentations, posters and journal articles while incorporating peer review feedback.
We've sorted each of our undergraduate, graduate and doctoral programs into unique Areas of Interest. Explore these categories to discover which programs and delivery methods best align with your educational and career goals.
Explore Health and Medicine at Quinnipiac
References
1. Ostrom QT, Gittleman H, Liao P, et al. CBTRUS Statistical Report: Primary brain and other central nervous system tumors diagnosed in the United States in 2010-2014. Neuro Oncol. 2017;19(suppl_5):v1-v88. doi:10.1093/neuonc/nox158
2. Larkin SJ, Ansorge O. Pathology and pathogenesis of craniopharyngiomas. Pituitary. 2013;16(1):9-17. doi:10.1007/s11102-012-0418-4
3. Castle-Kirszbaum M, Shi MDY, Goldschlager T. Quality of Life in Craniopharyngioma: A Systematic Review. World Neurosurg. 2022;164:424-435.e2. doi:10.1016/j.wneu.2022.05.038
4. Zheng Y, Ong SH, Vellayappan B, Nga VDW. Management of first recurrence or progression of craniopharyngioma after resection alone: A systematic review and individual-participant data meta-analysis. J Clin Neurosci. 2023;118:123-131. doi:10.1016/j.jocn.2023.10.014
5. Chowdhary A, Spence AM, Sales L, Rostomily RC, Rockhill JK, Silbergeld DL. Radiation associated tumors following therapeutic cranial radiation. Surg Neurol Int. 2012;3:48. doi:10.4103/2152-7806.96068
6. Sharifi A, Hwang PH, Kouhi A, Zojaji M, Ghaffari ME, Ghaedsharaf S. Role of Early Postoperative Measurement of Copeptin in Prediction of Diabetes Insipidus Following Pituitary Surgery in Adults: A Systematic Review Plus Meta-analysis. World Neurosurg. Published online October 28, 2024. doi:10.1016/j.wneu.2024.10.006
7. Miao Y, Fan K, Peng X, et al. Postoperative hypothalamic-pituitary dysfunction and long-term hormone replacement in patients with childhood-onset craniopharyngioma. Front Endocrinol (Lausanne). 2023;14:1241145. Published 2023 Nov 6. doi:10.3389/fendo.2023.1241145
8. Schroeder LE, Kritselis M, Lala N, Boxerman J, Alhusaini S. Pearls & Oy-sters: Adult-Onset Craniopharyngioma Presenting With Cognitive Dysfunction and Obstructive Hydrocephalus [published correction appears in Neurology. 2024 Jul 9;103(1):e209596. doi: 10.1212/WNL.0000000000209596]. Neurology. 2023;101(21):974-978. doi:10.1212/WNL.0000000000207857
9. Lin B, Xiang S, Chen J, et al. Assessment of quality of life in patients with craniopharyngioma and identification of risk factors for compromised overall wellness. Arch Endocrinol Metab. 2023;68:e230001. doi:10.20945/2359-4292-2023-0001
10. Bereket A. Postoperative and Long-Term Endocrinologic Complications of Craniopharyngioma. Horm Res Paediatr. 2020;93(9-10):497-509. doi:10.1159/000515347
11. Hald JK, Eldevik OP, Quint DJ, Chandler WF, Kollevold T. Pre- and postoperative MR imaging of craniopharyngiomas. Acta Radiol. 1996;37(5):806-812. doi:10.1177/02841851960373P275